Bariatric surgeon Richard Barbor recently spoke to TVNZ’s Breakfast show about the surge in popularity of weight loss drugs, Ozempic and Wegovy. Here is a condensed version of the interview.
Ozempic and Wegovy have gained fame for helping celebrities lose weight. However, the active ingredient in these medications, semaglutide, is primarily intended to treat type 2 diabetes. Their popularity as weight loss drugs has led to a global shortage, making them inaccessible to those who need them most and unavailable in New Zealand.
How does Ozempic work?
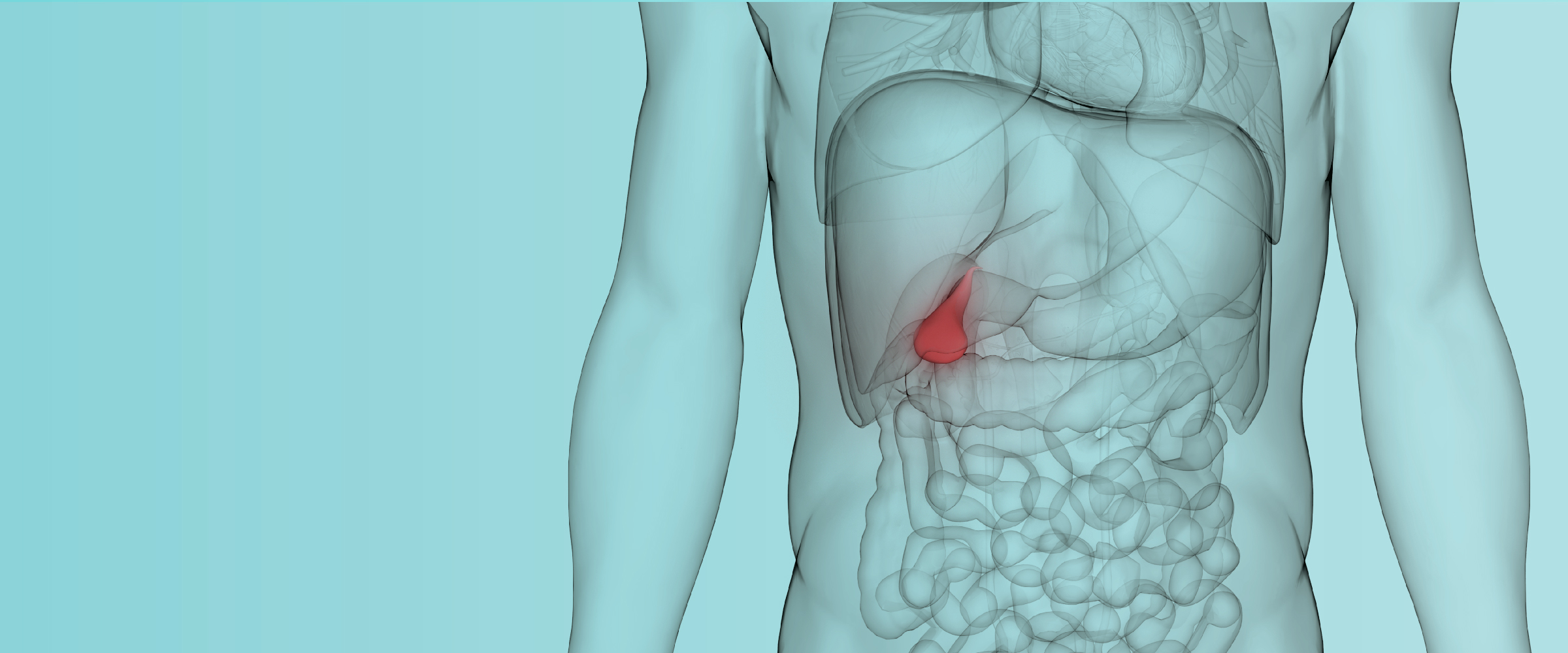
Ozempic is a “GLP-1 receptor agonist” that targets receptors in the brain, pancreas, and gut. GLP-1 receptor agonists mimic the GLP-1 hormone, helping to lower blood sugar levels and reduce appetite. This slows down the gut’s activity and makes the brain think you’re not hungry. Many patients report that they “just stopped thinking about food,” and if they did eat, they felt full almost immediately.
Are they miracle weight loss drugs?
No, they are not miracle drugs, but they are highly effective for treating type 2 diabetes. These medications are game-changers and do promote weight loss. They represent an important new class of medications that many people will use in the future. However, the associated weight loss is relatively modest, and weight can be regained once the medication is stopped. The hype surrounding these drugs, especially in Hollywood and media outlets like Oprah, is somewhat exaggerated.
Is that the reason for the shortage?
Yes, Ozempic must be one of the most Googled terms right now! The high demand has contributed to the global shortage.
Do we have Ozempic & Wegovy in New Zealand?
Currently, these medications are not available in New Zealand due to the global shortage. Manufacturers are working to increase production, so we expect to have them here eventually.
What are the alternatives?
In New Zealand, similar drugs like Saxenda are available. Saxenda works in a similar way but requires daily injections instead of the weekly injections that Ozempic requires. It is used for both type 2 diabetes and weight loss in New Zealand.
Learn more
Ozempic for Weight Loss: Richard Babor on Balancing the Promise and Perils